What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
Imaging Tests for Heel Pain

There are a number of imaging options for diagnosing heel pain. Heel pain can result from a variety of causes, and the choice of imaging method depends on the suspected condition. Common imaging tools for assessing heel pain include radiographs, diagnostic ultrasound, MRI, and CT scans. Radiographs are often used initially to rule out bone-related causes such as stress fractures or bone cysts. Different views, including lateral ankle and foot, calcaneal axial, and medial oblique views, can provide valuable information. Diagnostic ultrasound is a dynamic and cost-effective tool that offers detailed information about soft tissues, such as the plantar fascia, calcaneal bursa, nerves, and tendons. It is particularly useful for conditions like plantar fasciitis and Baxter's nerve entrapment. CT scans are less common but can be used when fractures are suspected. An MRI is the most comprehensive tool for diagnosing causes of heel pain, including plantar fasciitis, stress fractures, nerve entrapment, and soft tissue abnormalities. It can provide a detailed view of the heel region and associated structures. For specific conditions, a combination of ultrasounds and MRIs may offer the most comprehensive diagnostic approach. If you are suffering from heel pain, it is suggested that you make an appointment with a podiatrist for a proper diagnosis and individualized treatment plan.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of Foot Doctors of Utica. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
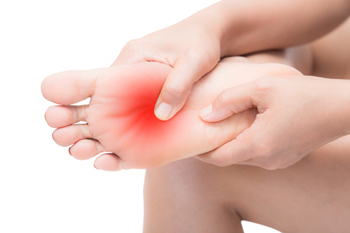
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our offices located in Herkimer, and New Hartford, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
Treatment Options for Achilles Tendonitis

Achilles tendonitis, inflammation of the long tendon at the back of the heel, can cause pain and restrict mobility. Typically stemming from overuse or excessive strain, this ailment can cause tearing of the tendon. Ceasing the activity that may have caused the injury is important, and keeping the weight off of that foot can help to reduce pain. Certain exercises can fortify the Achilles tendon, making it more resilient and improving its flexibility. Orthotic devices, such as shoe inserts, not only provide essential support to the affected tendon but also work to lessen undue strain. In certain cases, non-steroidal anti-inflammatory medication may be prescribed to alleviate pain and manage inflammation. For severe and persistent cases of Achilles tendonitis, advanced interventions such as corticosteroid injections may be considered. These treatments target inflammation and stimulate the body's natural healing processes. It is suggested that you make an appointment with a podiatrist for a comprehensive evaluation and personalized treatment plan for recovery from Achilles tendonitis.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Foot Doctors of Utica. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Herkimer, and New Hartford, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
See Your Foot Specialist Regularly If You Work On Your Feet
Charcot-Marie-Tooth Disease Impacts Functioning
Charcot-Marie-Tooth Disease, or CMT, is a disorder of the peripheral nerves, responsible for transmitting information to and from the brain and spinal cord. CMT disrupts these nerves, leading to sensory loss and muscle deterioration. This results in symptoms like balance problems, foot abnormalities, pain, and difficulty walking. Charcot-Marie-Tooth Disease is a progressive condition, worsening over time, and affecting about 150,000 people in the United States and 3 million worldwide. It is important to understand the peripheral nervous system to comprehend CMT. The peripheral nervous system links the central nervous system to organs, limbs, and skin, enabling the transmission of information and regulating functions like heartbeat and breathing. Nerve signals are carried by axons covered with myelin, akin to electrical wires in a home. CMT can cause myelin decay, slowing nerve signals and affecting longer limbs first. If you are having peripheral nerve damage affecting your feet, it is suggested that you make an appointment with a podiatrist for a proper diagnosis and treatment that will provide you relief with everyday functioning.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with one of our podiatrists from Foot Doctors of Utica. Our doctors will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Herkimer, and New Hartford, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Treatment and Recovery for a Broken Ankle

A broken ankle is a distressing injury that can occur from accidents or sudden trauma. There are three bones that make up the ankle joint, the tibia, fibula, and talus. One or more of these bones can become fractured, and often demands immediate medical attention. This is necessary to assess the severity and type of fracture, which can range from stable to complex. The treatment varies and can involve immobilization with a cast or splint, and sometimes surgical intervention with the insertion of pins or plates to realign the bones. Recovery times depend on the fracture's complexity and the chosen treatment. Generally, mild fractures may heal in six to eight weeks, while more severe injuries may take several months. Patience and adherence to medical advice are key during recovery, ensuring a return to normal activities with a healed and stable ankle. If you have fractured your ankle, it is suggested that you confer with a podiatrist who can determine what the best course of treatment is for you.
Broken ankles need immediate treatment. If you are seeking treatment, contact one of our podiatrists from Foot Doctors of Utica. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our offices located in Herkimer, and New Hartford, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Types of Hammertoe Surgery

Early intervention in managing painful hammertoes can prevent the need for surgery. However, for some individuals, surgery may become a viable option. It is important to address underlying factors such as rheumatoid arthritis prior to considering surgery. A number of surgical options are available, depending on the severity or advancement of the hammertoe. Tendon transfer, suitable for flexible hammertoes, involves repositioning tendons to improve alignment and appearance. Joint resection is beneficial for fixed hammertoes. This procedure consists of adjusting ligaments, tendons, and bone portions. Fusion is generally reserved for severe fixed hammertoes that may require this approach. Joint portions are removed to stimulate bone growth and straighten the toe. Toe removal is employed only in rare cases of extreme pain, although it comes with significant considerations. Surgery is often performed as an outpatient and can involve local anesthesia. Strengthening exercises and wearing proper footwear can help to aid in recovery. For guidance on managing a hammertoe, it is suggested that you consult with a podiatrist for treatment options.
Hammertoe
Hammertoes can be a painful condition to live with. For more information, contact one of our podiatrists from Foot Doctors of Utica. Our doctors will answer any of your foot- and ankle-related questions.
Hammertoe is a foot deformity that affects the joints of the second, third, fourth, or fifth toes of your feet. It is a painful foot condition in which these toes curl and arch up, which can often lead to pain when wearing footwear.
Symptoms
- Pain in the affected toes
- Development of corns or calluses due to friction
- Inflammation
- Redness
- Contracture of the toes
Causes
Genetics – People who are genetically predisposed to hammertoe are often more susceptible
Arthritis – Because arthritis affects the joints in your toes, further deformities stemming from arthritis can occur
Trauma – Direct trauma to the toes could potentially lead to hammertoe
Ill-fitting shoes – Undue pressure on the front of the toes from ill-fitting shoes can potentially lead to the development of hammertoe
Treatment
Orthotics – Custom made inserts can be used to help relieve pressure placed on the toes and therefore relieve some of the pain associated with it
Medications – Oral medications such as anti-inflammatories or NSAIDs could be used to treat the pain and inflammation hammertoes causes. Injections of corticosteroids are also sometimes used
Surgery – In more severe cases where the hammertoes have become more rigid, foot surgery is a potential option
If you have any questions please contact our offices located in Herkimer, and New Hartford, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.